Understanding Chronic Inflammatory Rheumatic diseases
Explore this health file to better understand Chronic Inflammatory Rheumatic diseases : its types, its causes, its symptoms but also the treatments
Posted on
I) Chronic Inflammatory Rheumatic diseases: definition
Chronic inflammatory rheumatic diseases (CIR) are diseases of the joints and/or spine that cause pain that can wake up at night and is usually worse in the morning than in the evening [1].
Chronic inflammatory rheumatic diseases include several different conditions such as rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, pseudo-rheumatoid arthritis and juvenile idiopathic arthritis. We will focus on the first three of these in this health dossier [1].
II) Rheumatoid arthritis
-
Definition
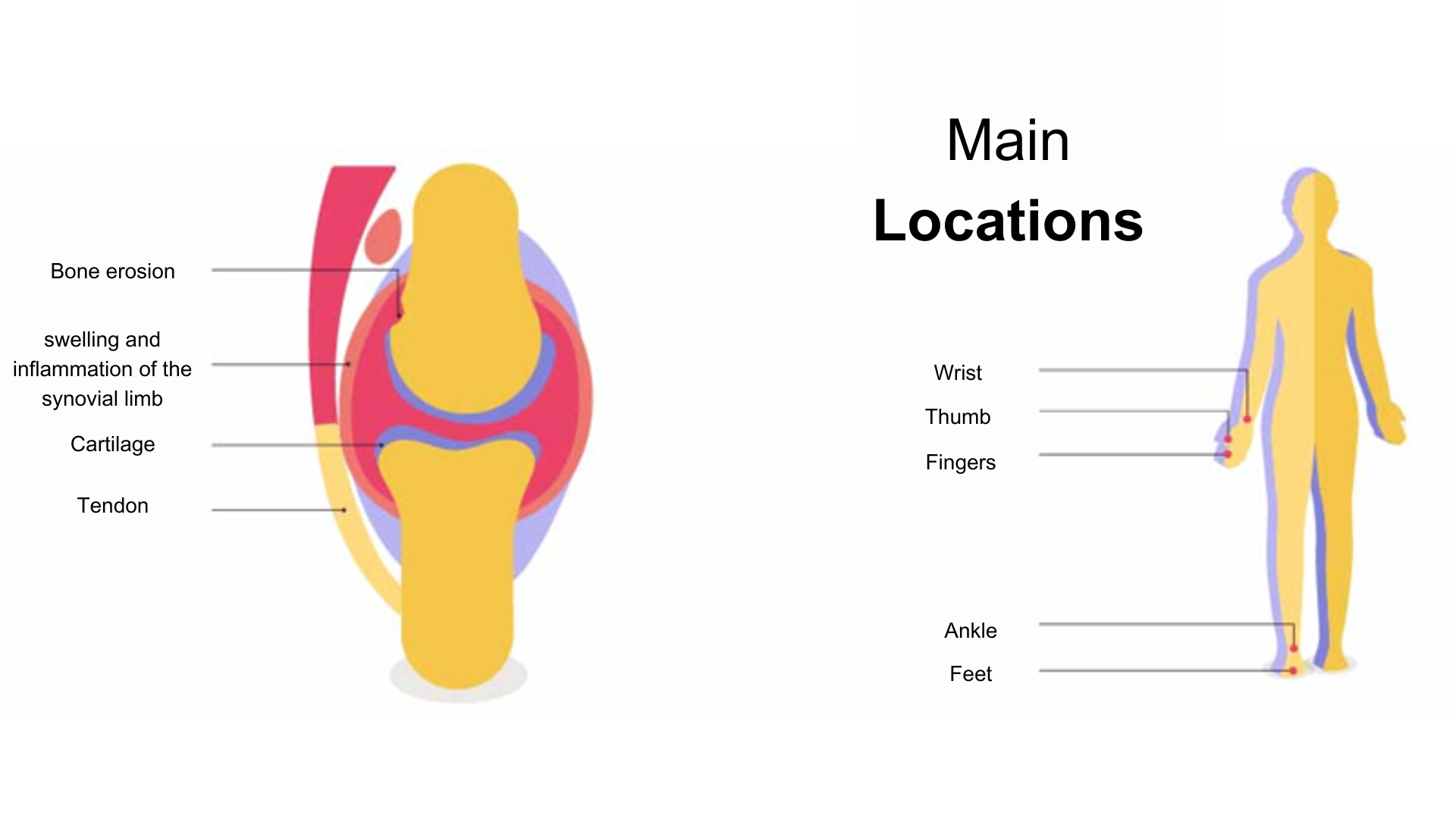
Rheumatoid arthritis is a severe inflammatory autoimmune disease that affects the joints: they gradually deteriorate and destroy, which can lead to disability.
Generally, rheumatoid arthritis begins with stiffness and swelling of several joints such as the wrists, hands, fingers, which causes pain. Symptoms are generally more present at the end of the night and in the morning.
These pains progress over time to more severe symptoms. [2]
-
Causes
The exact causes of rheumatoid arthritis (RA) are not fully understood. However, it is generally accepted that the disease may be favored by genetic predispositions and environmental factors.
Research has identified several genes that appear to increase the risk of developing RA, but they alone cannot explain the onset of the disease.
Indeed, it has been shown that environmental factors can also increase the risk of developing RA:
- Smoking: RA is more common, more severe and less responsive to treatment in smokers
- Gender: the disease is two to three times more common in women than in men
- Age: the disease usually appears around the age of 45 [2]
-
Symptoms
Rheumatoid arthritis often begins with painful stiffness in several joints, mainly the wrists, hands and fingers, which then become swollen. Being an inflammatory disease, symptoms are usually more pronounced late at night and early in the morning. The stiffness gets better after several minutes. In addition to the pain, fatigue, lassitude and loss of appetite may appear.
Treatments are most effective at this initial stage of the disease and offer promising results for the long term.
Thereafter, the disease evolves in painful attacks, interspersed with more or less complete remission periods. These painful attacks can affect all joints such as elbows, shoulders, neck, feet, toes, knees, hips and neck. At this stage, the evolution of the disease becomes visible on X-rays which show a destruction of the joints manifested by the pinching of the cartilages, the destruction of the neighboring bones and the dislocation of joints.
After several years, rheumatoid arthritis leads to joint deformities and tendon destruction that often require orthopedic surgery to repair or replace a joint with a prosthesis. [2]
[3]
-
Treatment
Rheumatoid arthritis is a severe but treatable inflammatory disease. In recent years, new treatments have been discovered that in most cases result in significant improvement in symptoms and sometimes prolonged complete remission.
As with many diseases, treatment is most effective if started early. It is therefore important to see a doctor quickly in case of joint pain or swelling.
To treat the pain, it is usually recommended to give the patient a painkiller, most often paracetamol.
To treat the inflammation, corticosteroids can be prescribed as they are effective at low doses. However, they must be monitored.
Finally, to deal with the immune disorder, an immunosuppressant (methotrexate) is also prescribed to the patient.
Once the treatment is initiated, monitoring should be done to ensure that the patient is tolerating the various medications and that they are effective.
If the disease progresses despite methotrexate, targeted therapies may be initiated. Each of these therapies targets a specific player in the inflammatory process. They result in a favorable response in ¾ of cases and prolonged remission in ¼ of cases. [2]
III) Ankylosing spondylitis
-
Definition
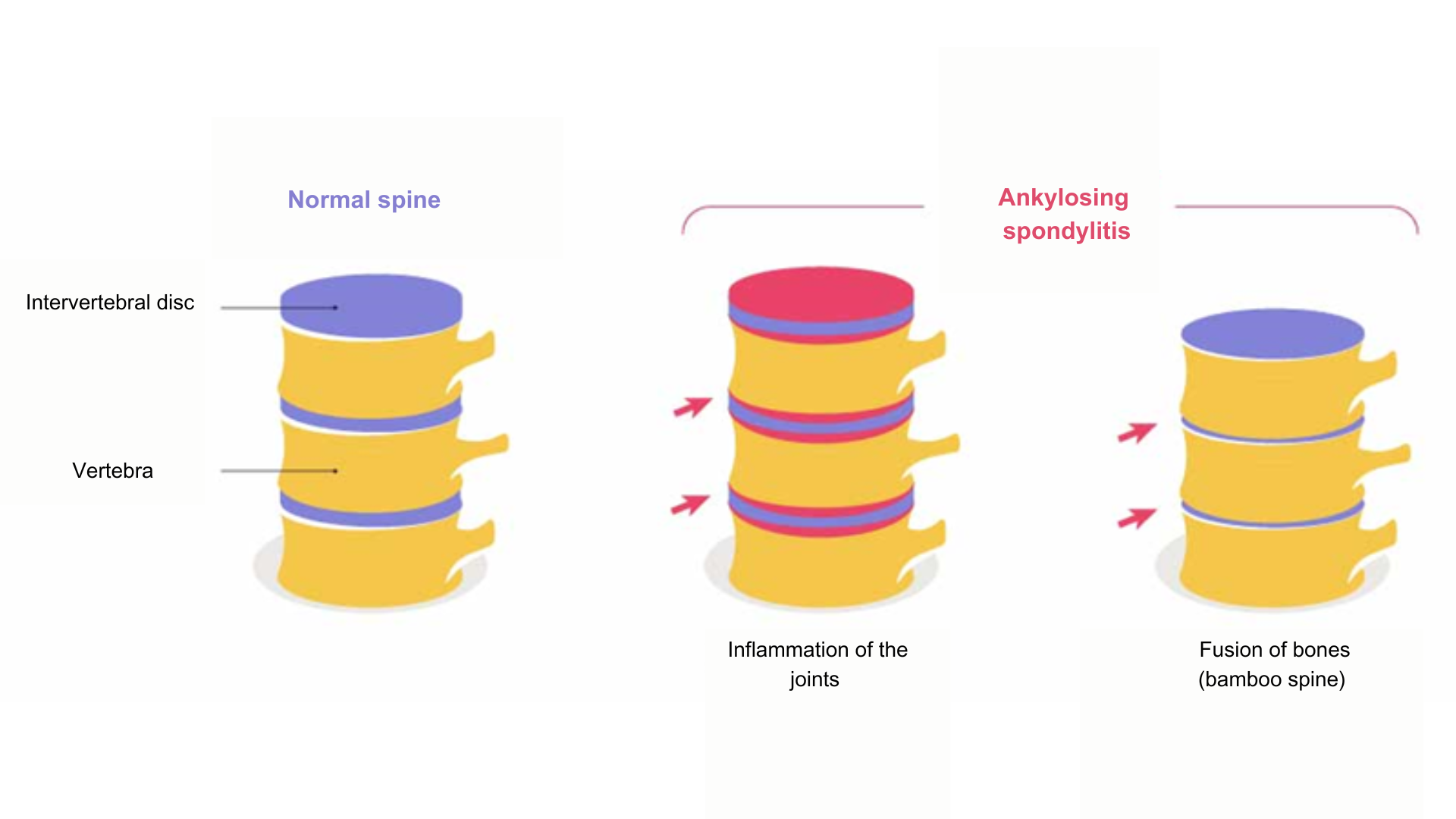
Ankylosing spondylitis (AS) is a chronic inflammatory disease that primarily affects the spine and sacroiliac joints in the pelvis. It manifests itself through painful flare-ups followed by periods of calm. It can sometimes progress to stiffening of the affected joints [4]
[5]
-
Causes
Although several contributing factors have been identified, the exact causes of ankylosing spondylitis (AS) remain unknown. However, genetic and environmental factors may play a role in the likelihood of developing the disease. [4]
Genetic background is an important factor to consider, as it is common for multiple members of the same family to have the disease.
A disturbance of the immune system, especially the presence of the HLA B27 gene, could also favor the development of the disease. [4]
Finally, environmental factors such as smoking and a lasting change in the intestinal flora have also been mentioned as potential factors that can favor the development of ankylosing spondylitis. [4]
-
Symptoms
The first signs of ankylosing spondylitis are characterized by attacks of back or lumbar pain (low back pain) that may seem trivial. These attacks last a few days to a few weeks and eventually get better. As the symptoms are not very precise and get better with time, the diagnosis can take time, up to eight years after the onset of the disease, thus delaying medical treatment [6].
Therefore, in case of spinal pain, certain symptoms should alert the patient to seek medical attention:
- Spinal pain is of “inflammatory” type: it tends to occur at night, waking the person up around two or three in the morning, and is not relieved when resting
- Pain occurs in one buttock, sometimes in both and sometimes “rocking”.
- One heel (or both) is painful (talalgia) in the morning when waking up, but the pain progressively diminishes when walking
- A finger or a toe starts to swell
- Stiffness in one or more other joints (knees, ankles, shoulders, etc.) is present in the morning when you wake up and lasts for more than half an hour
- The pain is associated with significant fatigue
- Painful attacks persist for at least three months and tend to last longer and longer [6]
-
Treatment
Comprehensive management of ankylosing spondylitis is aimed at treating pain, preventing joint stiffness and improving quality of life.
Non-steroidal anti-inflammatory drugs (NSAIDs) are often prescribed to control symptoms, especially pain, but their use must be limited because of their side effects. In case of intolerance or allergy to NSAIDs, painkillers such as paracetamol can be used.
If NSAIDs are ineffective or need to be discontinued temporarily, corticosteroids can be used to reduce inflammation.
If pain persists despite these treatments, other options (methotrexate, anti-TNF alpha, etc.) can be prescribed to reduce painful flare-ups and prevent disease progression.
Rehabilitation is also important to maintain joint mobility and prevent joint stiffening [7].
IV) Psoriatic arthritis
-
Definition
Psoriatic arthritis is a form of chronic inflammatory rheumatic diseases that is part of the spondyloarthritis type. It is caused by an immune system reaction against joints, tendons and ligaments. Although it is often seen in people with psoriasis, a chronic inflammatory skin disease, about 20% of people with psoriatic arthritis do not have this skin disease. [8]
-
Causes
Psoriatic arthritis results from a combination of genetic and environmental factors, as do psoriasis and other chronic inflammatory rheumatic diseases. Stress, physical or emotional trauma and infections are examples of environmental factors that can contribute to the development of this disease. Under the effect of these factors, the immune system can react abnormally and attack the tissues of the joints, considering them as foreign bodies. This immune response leads to local inflammation that causes joint pain, stiffness, and swelling, which can progressively cause damage. [10]
-
Symptoms
Psoriatic arthritis has nonspecific symptoms that may resemble those of other forms of chronic inflammatory rheumatic diseases. If the acute attacks of this disease are mild and widely spaced, the disease may go undiagnosed. Indeed, in half of the patients with psoriasis and psoriatic arthritis, the latter has never been identified. [11]
However, two characteristic symptoms of psoriatic arthritis are present in 30-50% of patients: enthesitis, which is inflammation of the attachments of ligaments and tendons to the bones, and dactylitis, which is inflammation of the joints of the fingers, causing pain and swelling. These symptoms are often asymmetrical, affecting only one side of the body. [11]
Other symptoms may also be observed such as joint pain that wakes up in the middle of the night, fatigue, especially during attacks, morning joint stiffness that is relieved by movement, and swelling in the joints due to inflammation of the synovial membrane [11].
-
Treatment
Acute attacks of psoriatic arthritis are often treated with non-steroidal anti-inflammatory drugs (NSAIDs).
Analgesic drugs may also be prescribed to relieve pain, but only for a limited time. If necessary, corticosteroid injections may be given directly into the affected joints to reduce inflammation.
If treatments to relieve flare-ups of psoriatic arthritis are not sufficient, other options can be considered by the physician. [12]
Discover our health files by clicking here.
POI 0843-04/23
Sources:
[1] https://www.chu-rouen.fr/rhumatismes-inflammatoires-chroniques/#:~:text=Qu’est%20ce%20qu’un,le%20matin%20que%20le%20soir.
[2] https://www.inserm.fr/dossier/polyarthrite-rhumatoide/
[3] https://ucbcares.fr/patients/rhumatismes-inflammatoires-chroniques/fr/content/1259231040/polyarthrite-rhumatoide
[4] https://www.ameli.fr/assure/sante/themes/spondylarthrite-ankylosante/definition-facteurs-favorisants
[5] https://ucbcares.fr/patients/rhumatismes-inflammatoires-chroniques/fr/content/932373360/la-spondyloarthrite-axiale
[6] https://www.ameli.fr/assure/sante/themes/spondylarthrite-ankylosante/symptomes-diagnostic-evolution
[7] https://www.ameli.fr/assure/sante/themes/spondylarthrite-ankylosante/traitement-medical
[8] https://www.vidal.fr/maladies/appareil-locomoteur/rhumatisme-psoriasique.html
[9] http://marker.to/Dw4hrE
[10] https://www.vidal.fr/maladies/appareil-locomoteur/rhumatisme-psoriasique/causes.html#:~:text=Comme%20le%20psoriasis%20et%20les,ou%20%C3%A9motionnels%20ou%20des%20infections).
[11] https://www.vidal.fr/maladies/appareil-locomoteur/rhumatisme-psoriasique/symptomes-diagnostic.html
[12] https://www.vidal.fr/maladies/appareil-locomoteur/rhumatisme-psoriasique/medicaments.html#:~:text=Les%20pouss%C3%A9es%20de%20rhumatisme%20psoriasique,prescrits%20pour%20une%20dur%C3%A9e%20limit%C3%A9e
